Click here to see all images
December, 2024
Case of the Month
Clinical History: A 35-year-old man, former light smoker (2 pack-years), with a history of tuberous sclerosis and amyloidosis with associated end-stage renal disease, presented with multiple bilateral ground glass pulmonary nodules detected on a chest-CT scan, which was done as part of renal transplant work-up. A right upper lobe wedge resection was performed (see figures 1 through 4).
Q1. What is the nature of this lesional process?
- Neoplastic-benign
- Infectious
- Hamartomatous
- Neoplastic - malignant
Q2. Which finding is commonly associated with this diagnosis?
- Diffuse idiopathic pulmonary neuroendocrine cell hyperplasia (DIPNECH)
- Lymphangitic carcinomatosis
- Bronchiolocentric non-necrotizing granulomas
- Lymphangioleiomyomatosis
Q3. Which of the following best describes the histologic features of this lesion?
- Enlarged cells with increased nuclear-to-cytoplasmic ratio
- Cuboidal cells with minimal cytologic atypia
- Cuboidal-to-columnar cells with apical snouts
- Lack of elastic fibers within septae
Answers to Quiz
Q2. D
Q3. B
Diagnosis
Discussion
Though MMPH is typically asymptomatic, some patients may report non-specific respiratory symptoms or present with pneumothorax. More commonly, the diagnosis is incidental, with the lesions first described during imaging performed for other reasons. The condition is generally indolent and lung lesions are not progressive. Treatment or follow-up imaging are therefore unnecessary.
On high resolution chest CT imaging, MMPH is characterized by scattered sub-centimeter ground glass opacities with no regional predilection. This radiographic finding is not diagnostic of MMPH and can be seen in multiple malignant and non-neoplastic processes, including multifocal atypical adenomatous hyperplasia, lymphangitic pulmonary metastases, and granulomatous reactions. However, in the correct clinical setting, particularly with a known history of TS, the radiologic picture of multiple randomly distributed ground glass nodules should raise the consideration of MMPH.
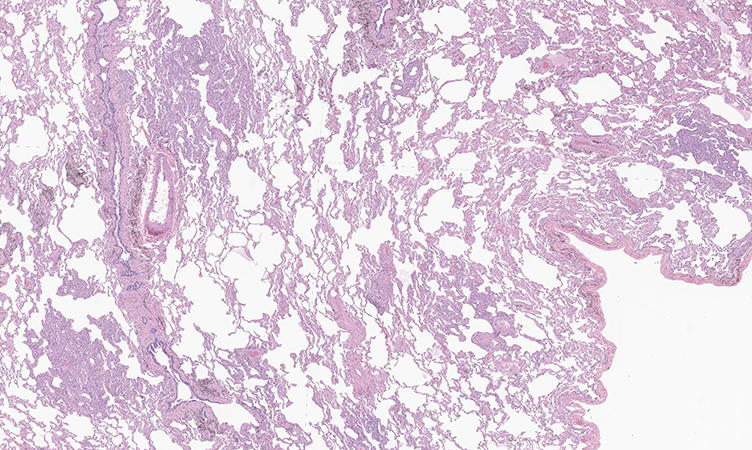
Histologically, MMPH consists of multicentric, nodular, well-defined proliferations of cuboidal pneumocytes along the alveolar walls (figures 1 and 2). The pneumocytes exhibit only mild cytologic atypia with preserved nuclear to cytoplasmic ratios (figures 3 and 4). Septal thickening associated with increased elastic fibers is a characteristic finding and can be highlighted with the use of elastic fiber staining. TTF-1 and Napsin A immunohistochemical stains are positive, consistent with the pneumocytic origin of MMPH, but melanocytic (HMB45, MelanA, MITF) and hormonal (ER, PR) markers are negative, unlike in LAM.
MMPH has a significant radiographic and histologic overlap with atypical adenomatous hyperplasia (AAH). Therefore, the clinical presentation is a key factor in distinguishing the two entities; while MMPH should be suspected in TS patients, AAH is commonly seen in the background or setting of a lung neoplasm. Though there is a certain degree of histologic overlap, essentially, type II pneumocytes in MMPH show abundant cytoplasm with unremarkable nuclei, whereas the pneumocytes in AAH exhibit higher nuclear to cytoplasmic ratio and worse nuclear atypia. Additionally, the septal thickening in MMPH is often characterized by elastic fiber hyperplasia.
Take home message for trainees: Multifocal micronodular pneumocyte hyperplasia (MMPH) is a hamartomatous pneumocyte proliferation associated with tuberous sclerosis. The lesions classically present as multifocal ground glass opacities and microscopically consist of nodular pneumocyte proliferations with mild cytologic atypia. The morphologic overlap with atypical adenomatous hyperplasia is a potential diagnostic pitfall.References
Konno S, Shigemura M, Ogi T, et al. Clinical Course of Histologically Proven Multifocal Micronodular Pneumocyte Hyperplasia in Tuberous Sclerosis Complex: A Case Series and Comparison with Lymphangiomyomatosis. Respiration. 2018; 310-316.
Popper HH, Juettner-Smolle FM, Pongratz MG. Micronodular hyperplasia of type II pneumocytes--a new lung lesion associated with tuberous sclerosis. Histopathology 1991; 347-54.
Ristagno RL, Biddinger PW, Pina EM, et al. Multifocal micronodular pneumocyte hyperplasia in tuberous sclerosis. AJR Am J Roentgenol. 2005; 184(3 Suppl):S37-9.Contributors
Thoracic Pathology Fellow
Memorial Sloan Kettering Cancer Center, NY
Maelle Saliba, MD Thoracic Pathology Fellow
Memorial Sloan Kettering Cancer Center, NY
Marina K Baine, MD, PhD
Assistant Attending Pathologist
Memorial Sloan Kettering Cancer Center, NY